Learning to Listen: How Tracking Health Metrics Can Empower Vasculitis Patients
If there’s one thing vasculitis has taught me, it’s that paying attention to your body can help save your life. As a rare disease patient you have to learn to communicate with your doctors exactly how you are feeling. Missing a symptom or side effect can impact your treatment. Keeping tabs on all the medications, appointments, side effects, and symptoms can seem like a full-time job. Living in this unpredictable state means learning to ride the waves, but it also means learning how to track patterns—because the more you understand about your body, the better you can manage your health.
As an endurance athlete growing up, I learned how important tracking splits and times were to my progress. Now as a coach I use all that data to help guide athletes on their running journey. I brought that same mentality to my vasculitis treatment journey. My doctors became my new coaches. Their medication protocols became my new training plan. Keeping track of how I was feeling and being able to accurately relay that to my doctors helped ensure that I was getting the best care I could. The goal of this article is to help you understand why tracking information can help you on your vasculitis journey. It’s not just about writing down numbers or logging symptoms for the sake of it. It’s about giving yourself (and your doctors) more tools to make better decisions. It’s about learning to recognize the signs before a flare-up takes you out. It’s about understanding what helps make you feel better—and what doesn’t.
Why Tracking Matters
Vasculitis is different for everyone. Some of us deal with fatigue that won’t quit, while others battle joint pain, organ complications, or side effects from medications. With so many moving pieces, it’s easy to get lost in the chaos. But when you start tracking key health metrics, it makes it possible to track patterns as they begin to emerge. You start seeing connections between what you eat and how you feel, between how much you sleep and your pain levels, between stress and disease activity.
In the first few years after my diagnosis, it was dizzying attempting to put my life back together and make heads or tails of what mattered. All I knew was to follow the doctor's orders. But as things started to settle, I tried to rely on memory alone to keep track of how I was doing. But after my first relapse I realized I needed to take things a lot more seriously. When you’ve been in a lot of pain, you’ve been sleeping 16-18 hours a day, and days seem to run together, I found myself struggling to answer my doctor’s questions. As my doctor asked more and more specific questions, I realized how much I didn’t know. And that meant my doctors didn’t have the full picture either.
Being mindful of my symptoms daily and tracking important symptoms like I used to track my running splits gave me solid information to work with—not just blurry memories. More importantly, it helped me understand my own body in ways I never had before.
What to Track
If you’re new to tracking, it can feel overwhelming. There are a million different things you could keep tabs on, but you don’t have to track everything all at once. The key is to focus on the areas that impact your quality of life the most. Here are a few metrics that have helped me:
1. Fatigue Levels
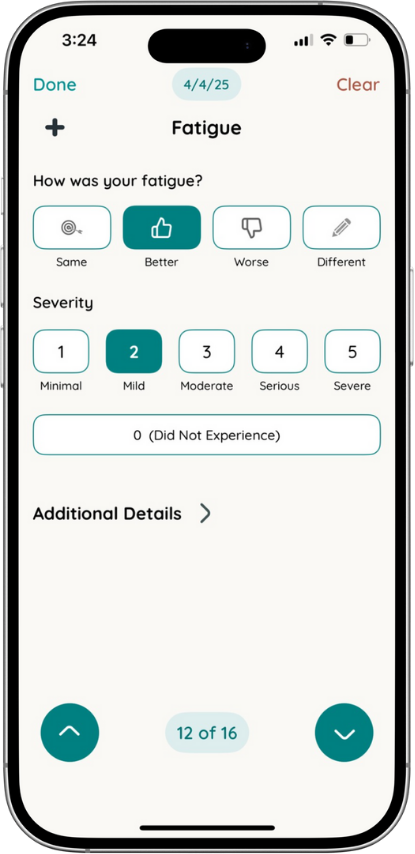
Fatigue is one of the hardest symptoms to describe because it’s so much more than just being tired. Keeping a daily log of my energy levels (on a scale of 0-5) helped me notice patterns I hadn’t seen before. For example, I started to realize that on weeks when I wasn’t hydrating well, my fatigue was worse. Knowing that helped me take better care of myself.
2. Pain and Inflammation
Tracking where and when I experience pain has been a game-changer. Writing down when my joints are stiffest or when my muscle aches are at their worst helps me and my doctor understand how my disease is progressing. It also helps me recognize if a new treatment is working.
3. Medication Side Effects
Medications come with a long list of potential side effects, and it can be tough to know which ones are actually affecting you. By logging any nausea, dizziness, headaches, or other changes, I’ve been able to figure out which side effects are worth pushing through and which ones need to be addressed.
4. Sleep Quality
Poor sleep can make everything worse. I started tracking my sleep hours and how restful I felt in the mornings, and it became clear that stress was playing a bigger role than I realized. Once I started prioritizing relaxation before bed, my sleep improved—and so did my overall well-being.
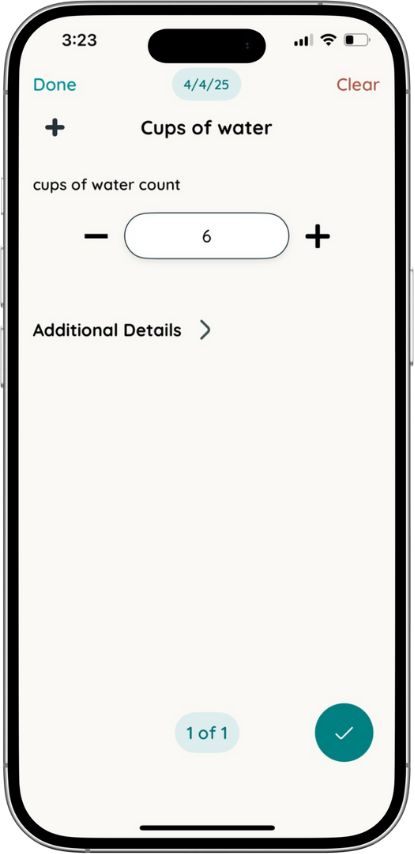
5. Nutrition and Hydration
I never used to think much about how my diet affected my vasculitis. But when I started logging what I ate and drank, I noticed some surprising trends. Skipping meals led to more fatigue, and not drinking enough water left me feeling achy and sluggish. Small adjustments made a big difference.
6. Stress and Mental Health
Living with a chronic illness isn’t just physically exhausting—it’s mentally draining, too. Tracking my stress levels and mood fluctuations helped me realize that high-stress weeks often coincided with flares. That awareness pushed me to make mental health just as much of a priority as my physical health.
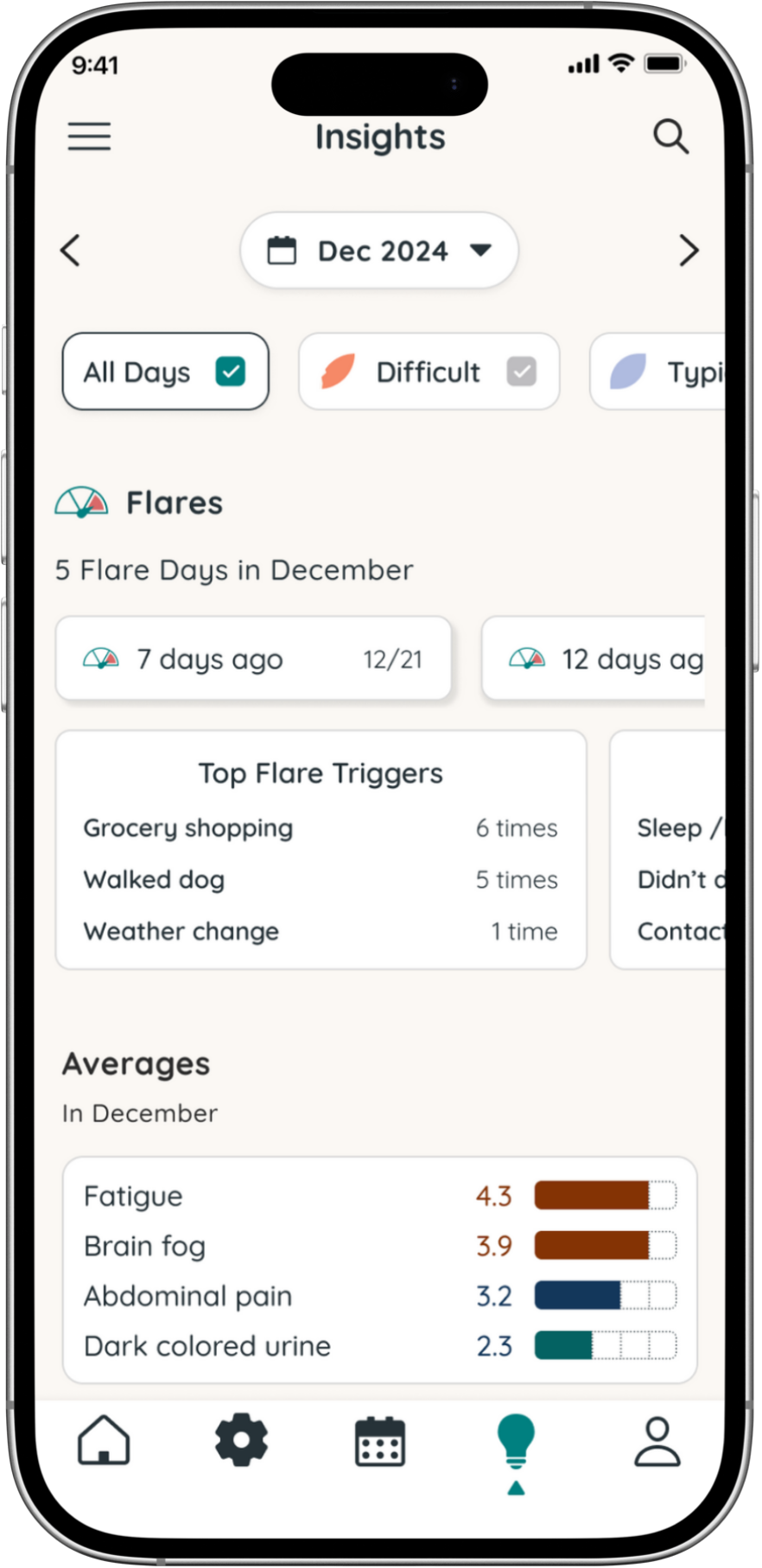
The Power of Patterns
The real magic of tracking is that it helps you connect the dots. When you have months’ worth of data, you can look back and see patterns you might have otherwise missed. Maybe you notice that your flares tend to happen after particularly busy weeks. Or that your fatigue worsens when your iron levels are low. These insights help you make proactive changes rather than always playing defense.
And it’s not just about personal insights—tracking also makes medical appointments more productive. Instead of walking in and saying, “I’ve been feeling off lately,” I can say, “Over the past three weeks, my fatigue has been at a 4 or higher most days, and my joint pain has increased after taking my medication at night.” That level of detail helps my doctors fine-tune my treatment plan and catch potential problems early.
Finding the Right Tracking System
There’s no one-size-fits-all approach to tracking. Some people prefer old-fashioned notebooks, while others use spreadsheets or apps. The key is to find a system that’s easy to stick with. That’s why I’m excited about tools like Folia Health’s app, which makes tracking and sharing health data with doctors simpler than ever. Having all my health information in one place takes the guesswork out of managing my disease.
Exercise as a Key Metric
As a running and health coach with a master’s degree in exercise science, I’ve always understood the importance of movement. But living with vasculitis has taught me just how valuable exercise tracking can be. Keeping tabs on my activity levels, heart rate, and recovery has helped me navigate my disease in a way that makes sense for my body. Some weeks, I can push a little harder, while other times, I have to scale back. Tracking my workouts alongside my symptoms has given me a better sense of when I’m thriving and when I need to slow down. It’s another layer of self-awareness that helps me stay in control of my health.
Learning to Listen to Your Body
At the end of the day, tracking is just a tool—it’s not a cure, and it won’t eliminate the unpredictability of vasculitis. But what it can do is help you become an expert on your own body. The more you understand about what makes you feel better or worse, the more control you have over your own health.
Vasculitis will be a lifelong battle, but that doesn’t mean we have to be passive bystanders. By learning to listen to our bodies and tracking what matters, we can take a more active role in managing our health—and that’s a power worth embracing.
About the Author:
Brandon Hudgins is a retired pro distance runner and co-founder of High Point Athletic Club (HPAC), a coaching organization based in High Point, NC. With over 10 years of experience, he trains athletes of all levels across the U.S.
Brandon holds degrees in Physical Education and Exercise Science and is the author of Going the Distance and several research publications.
Diagnosed at 21 with Granulomatosis with Polyangiitis (GPA), a rare form of vasculitis, he overcame major setbacks to qualify for the 2016 U.S. Olympic Trials. His journey led to the launch of Victory Over Vasculitis, a national awareness campaign turned full-time program in 2024. Through coaching and advocacy, Brandon inspires others to keep pushing—no matter the odds.