The Leaflet: Folia User Newsletter
Keep up the Folia Community, research happenings, and other insights
** If you are already part of the Folia community, no need to input your email!
October 2023
Fall into the new season with the latest updates on the Folia tracking experience, community-driven research initiatives, and Folia user community!
This Quarter’s latest news
Little insights into what’s been happening at Folia!
Redesign Launch
It’s been 5 years in the works and we are so excited to share that the new Folia 2.0 is live on all platforms! We’ve been listening to your feedback and suggestions to make sure we are delivering the best tracking experience yet. Here is what you can expect from our latest update:
Home Screen & Daily Journal: A new look to your home base with everything you need in one place
Observation Tracking: Accurately log your symptoms in great detail in under a minute
Treatment Tracking: Group your treatments together and easily track with a single click
Flexible Scheduling: Set up any schedule you’d like for your treatments
Tag Tracking: Capture important details about your health with consistency via tags
Flare Tracking: Report significant health events with our smart Flare Tracker
We are always open for suggestions from our users as we continue to add new features. If you are unsure or having difficulties navigating the new update, we are here to help! Send us a message in the app or email us at [email protected] and the team will reach out as soon as possible.
Exciting new updates and integrations are still to come and you will be the first to learn more about it!
A special shoutout to our Engineering team who has worked tirelessly for the big launch! Check out the Folia Spotlight section of this Leaflet to learn more about all our fantastic engineers :)
Canopy Series wrap up
We kicked off 2023 by asking you what questions you have about how others manage their health. We all experience this world differently. We also all experience our health differently. This is not to say that we don’t have similar experiences, and can’t learn from each other. By coming together and creating the Canopy Series, we collectively created a new approach to understanding the landscape of specific conditions, and what daily life can look like.
Sometimes, asking questions can lead to more questions. So what is next? Creating more reports in more conditions. Knowledge should not be a limited resource, and should instead be shared with the community.
Check out insights from our Canopy Series on our website!
Strengthening our communities
One of our goals is to create these reports in three specific communities we have been working so hard to build. We have been focusing on building communities with individuals who have or care for someone who has Multiple Sclerosis, Huntington’s Disease and Myasthenia Gravis.
These are three different conditions, as Huntington’s is an inherited progressive neurodegenerative disease, MS is a disease of the central nervous system, and Myasthenia Gravis is an autoimmune condition. These conditions affect individuals in a wide range of ways, and require the Folia app to be as flexible as possible to make sure individuals capture and are able to understand the data they need. Through the redesign process we have learned so much from individuals in the community, and we look forward to the continued conversations.
If you are or know someone with one of these conditions, please reach out in app or via email to [email protected]. We would love to provide a platform to share your story.
User Community Spotlight
Jenna is a 41 year-old veterinarian technician living in New Jersey. Unlike most cystic fibrosis (CF) patients who are diagnosed either at birth or in their early years of childhood, she was “late to the game” and didn’t receive a proper diagnosis until 12 years old. Jenna was dealing with a lot of medical problems leading up to her medical diagnosis – she frequently had coughing exacerbations, her fingers would turn blue for no reason, and experienced severe asthma allergy attacks. “It felt like I lived at the pediatrician’s office,” Jenna shares. The biggest concern was that she couldn’t maintain any body weight, and so her mom looked up an allergist to take a further look at Jenna’s symptoms. With one look, the allergist said Jenna either had pneumonia or CF. Shortly after, Jenna got her sweat and genetic testing done and was officially diagnosed with CF. That one doctor’s visit changed Jenna’s entire life.
“Navigating life is one thing. Navigating life with a chronic illness is a whole other challenge.” It felt like Jenna was playing catch up – since she went undiagnosed for so long, she had “12 years without any medical treatments or dietary supplements to make up for.” This period also coincided with her teenage years. She’d go through coughing exacerbations during class and would go to school with long sleeves to cover all the IV treatments she was getting in the nurse’s office. “I was so embarrassed, I would feel the need to explain my conditions to everyone.”
Conditions like CF have an added layer of complexity because not all symptoms are visible to others, and sometimes you don’t look the part of a ‘typical patient’. CF patients may qualify for disability benefits due to their lung and pulmonary symptoms. For example, Jenna has a handicap parking placard that she uses, but rather than easing stress, it can add to the complexities of living with a condition. “The looks that I get when I park at the store or amusement park. They don’t say anything, but you can feel the judgment,” she shares. “People look at you weird. You’re too young, you don’t have a walker, you clearly aren’t a senior citizen.”
It’s a narrative that Jenna battles with herself too. “When I look at myself, I look normal, but inside it’s a jumbled mess.” It’s a strange and complex illness to characterize, since it can vary so much day to day. There are days where Jenna struggles to breathe – a short walk can lead to her heart pounding or her getting wheezy. Then, there are days when Jenna “feels like [she] doesn’t have CF at all, like [she] could run a mile.”
Jenna’s CF journey has had its ups and downs. “I’d get PICC lines every couple years, and a seasonal dose of antibiotics every fall.” Her condition mainly affected her joints, and she was diagnosed with osteoarthritis. Her care team suspects that all the years playing catch up on treatments caused the steroids to affect her joints and bones. Over the years, Jenna wanted a fresh view and a different perspective for her CF care. She found a team close to where she currently resides and called to ask if they were taking new adult CF patients. When they told her yes, Jenna started crying on the phone immediately out of relief.
“My new care team has just been instrumental to my health, both treating my physical symptoms and also keeping me mentally calm.” Jenna’s doctors empathize with her condition, telling her that it’s okay to need steroids or be on antibiotics. The center just opened in 2016 and is up-to-date on the newest treatments and has their own assistance program to help patients advocate for their health insurance. For Jenna, and for most patients getting care in the US, the ongoing financial battle with health insurance has always been draining. “You fight so hard to wake up everyday, and then you also have to fight to get the medicine to just be able to breathe? I had more fight in me when I was young, but now luckily my care team fights for me.”
It was also through her new CF clinic that Jenna found Folia about 2 years ago. Jenna took part in Folia’s year-long observational study to characterize the day-to- day symptoms of CF patients. She still keeps in touch with some study participants she’s met through the program and checks in with them every so often. “As I get older, I find it so important to be able to have these open-door, light hearted conversations with the people that just get it.” Jenna expresses how refreshing it is to have an outlet to share and connect with people who are going through the same journey that she is.
All throughout Jenna’s life and diagnostic journey, her support system has been a crucial part. “My family has moved heaven and earth to get the best care for me.” In school, her friends and the staff were wonderful and understanding. At work, her coworkers show their support by running a donation drive for CF initiatives every year. Through CF study initiatives and Facebook groups, she is inspired to share her story and connect with others. No one requires Jenna to explain herself or her conditions – they empathize with her struggles, support her during her bad days, and are always willing to learn.
Jenna doesn’t let her condition define her life – “I have so much more to give!” Her work and personal life has started to even out now. She’s a recent homeowner, where she wakes up every day excited to look out the window for deers and play with her four cats. She looks forward to traveling in the near future to see more of the world and to have a “mental and spiritual reset.” Her top destinations are her happy place at Disney, back to the Bahamas to swim with the wild pigs in Exuma Bay, and to check off her life-long bucket list of seeing the Northern Lights.
Folia Spotlight - Engineering Team
Folia Digest - Inverse Vaccines
Our immune system is a vital part of our health. This complex network of organs, cells, and proteins work to detect, defend, and remember foreign bodies. It recognizes infections, fights off viruses and bacteria to protect our body’s healthy cells. In the immune system, specialized T cells keep a record of all the pathogens it has fought off for future reference.
Autoimmune diseases occur when our body fails to tell the difference between our own and foreign unhealthy cells and so our immune system mistakenly attacks itself. The T cells work to retain a memory of the immune response, so this unintended process can happen even quicker in the future and is hard to control and treat. Currently, treatments for autoimmune diseases generally focus on suppressing the immune system’s activity as a whole. While this can mitigate the unintended attacks against our body’s healthy cells, it also leaves ourselves vulnerable to actual foreign viruses and bacteria.
What if there was a way for our immune system to stop remembering these false attacks on our own healthy cells? This could be a better way to treat autoimmune diseases – telling our body to stand down in response to “safe” cells while still allowing the immune system to respond to foreign pathogens at full force. A group of researchers at the University of Chicago are working on an “inverse vaccine” that could make this a reality.
How does it work?
Traditional vaccines work to introduce foreign antigens into the body to raise a slight alarm and prime our immune system to respond. The so-called inverse vaccine would just do the opposite. Instead of alerting the immune system, it suppresses the immune response by marking these antigens as “safe”.
The inverse vaccine leverages the ability of a special group of cells in our liver specialized to recognize our own healthy cells from foreign viruses and bacteria. The research team identified that tagging molecules with a special sugar called N-acetylgalactosamine (pGal) allows them to mimic this process. The immune system can learn that any antigens coupled with pGal are “safe cells”.
As outlined in the published paper, researchers tested out this hypothesis in the lab on mice with a type of multiple sclerosis, where T cells attack a specific antigen in myelin sheaths of the nervous system. The inverse vaccine tagged this antigen with pGal and was able to reprogram the animal’s immune system to recognize myelin cells as “safe”, suppress the immune attacks, and reverse the disease symptoms in the animal.
So what does this mean?
These findings on the inverse vaccine offer a promising solution for better therapies for autoimmune diseases. However, there is a long road ahead before these therapies are available on the market. There will have to be more research efforts to identify the molecular basis of various autoimmune diseases. Additionally, translating the success from animal models to a diverse and ever-changing human patient population will be tricky. Clinical trials for this type of inverse vaccine have already been launched for multiple sclerosis and celiac disease, and these results will be interesting to follow.
The lead researcher of the aforementioned paper, Jeffrey Hubbell, shares his excitement about what this means for the medical field – “What is so exciting about this work is that we have shown that we can treat diseases like multiple sclerosis after there is already ongoing inflammation, which is more useful in a real-world context.”
Read more about the inverse vaccine in their press release and published paper.
Past Editions
April 2023
Spring is blooming, and so is our Canopy Series research project! Learn about this, and learn from individuals who have participated in clinical trials.
Introducing: Peter
This quarter, we are excited to introduce Peter, our Director of Engineering. Peter currently lives in Texas with his girlfriend, Mari, and during the workday, codes and takes meetings with the company of his dog, Julie.
Peter was an original member of the Folia team, and joined because he believes in Folia’s positive mission. His favorite part of his job is the interesting challenges that arise with the engineering aspect of Folia’s platform. He enjoys working with the team because he knows everyone is doing something different, but they bring their skills to the table to contribute together. If he could do any other job at Folia, he would take on the role of Data Analysis.
An average Saturday for Peter typically involves a run with Mari, and a fun dinner somewhere in his new town. His favorite TV shows are Curb Your Enthusiasm and the Great British Baking Show.
This Quarter’s Latest News
Little insights into whats been happening at Folia!
Canopy Series
This season, we have been all about asking questions. Specifically, asked you what questions you have! We compiled the results from the surveys that have been completed, and came up with general questions that can be answered by tracking your health.
At the end of Canopy Series, you will receive a report that answers these questions and shows how other people are utilizing Folia to track their symptoms and treatments. Are you curious how other individuals with your condition are managing their treatment options? This is the type of question that we aim to answer through this research series.
If you are on a diagnostic odyssey and don't yet have a diagnosis, don't worry! We will provide you an opportunity soon to have your questions answered.
Sjögren's Awareness Month
April is Sjögren's Syndrome awareness month. We have such a wonderful community of individuals with Sjögren's, and we will be sharing their stories on our blog all month.
If you have a story you would like to share, we would love to feature you. You can have any diagnosis, be a caregiver, or be on a diagnostic odyssey - we love learning from everyone.
Community Spotlight: The things they don't tell you about participating in a clinical trial.
What if you grew up knowing you wouldn’t live to 50? How would you make a decision to join a clinical trial to potentially elongate your life? These thoughts and decisions aren’t foreign to individuals with Cystic Fibrosis.
In 2017, researchers stated that the median predicted survival age for individuals born between the years of 1993 and 1997 with Cystic Fibrosis would live to 31 years old.
Jennifer’s Story
Jennifer was diagnosed with CF at age 37, and was born in 1965. To say she is defying the odds is an understatement.
When Jennifer was born a mere 58 years ago, they didn’t know about her genetic mutation of CF. In fact, doctors and researchers didn’t know CF could be a product of a genetic mutation. Over the course of her first 37 years, Jennifer experienced various symptoms, but no one was able to put them together and recognize a root cause of her experiences.
At the age of 11, she had scoliosis surgery - a Harrington rod was placed in her back to fix the curvature of her spine. Nowadays, doctors are understanding a link between scoliosis and CF. After her surgery, she started experiencing pancreatic issues. Her doctor thought he fused a nerve to the pancreas during her scoliosis surgery. To address this issue, she was put on a diet to help manage pancreatic insufficiency. This is another telltale sign of CF - yet it would be many years before a pulmonologist put the pieces together and recognized she has CF.
Jennifer’s clinical trial journey hasn’t always been positive, yet she continues to advocate for their participation. With one trial treatment, she became diabetic. With another, she experienced a severe infection. Yet, she continues to partake in whatever she can, and she has fun while doing it. During one trial, she was inpatient at the hospital on the cardiac floor. She created a walking club for any patient on the floor who needed to walk the halls.
Most recently, Jennifer has been exploring clinical trials for Colonoscopies. Recent research suggests “The risk for colorectal cancer in adults with cystic fibrosis is 5–10 times greater than the general population, and even higher for people with CF who receive a lung or other solid organ transplant”. However, getting a colonoscopy is no easy feat for patients with CF. It involves a 5 day prep period, and last time Jennifer did this, her health deteriorated.
And so, Jennifer continues to contribute to research by participating in any and every study she can qualify for. Here is advice Jennifer has for anyone considering participating in a trial:
This is your opportunity to better the experience for the next generation.
You will learn something new every time you participate in something new, and this is priceless.
Sometimes it is hard to not know exactly how you are contributing to the study, but that’s okay! If you are okay with not knowing, then you won’t be disappointed.
Be open to doing whatever they need you to do. If they need to take labs, be okay with that.
Being part of a trial is so life changing because you are doing something to leave your little mark on the planet. It may not feel like it, but you are.
DeAnna was diagnosed with CF at 6 months, when she was classified as “failure to thrive”. She went through the motions of having CF for the first 22 years of her life without a hitch. Then, the hospitalizations began. They started happening yearly, and then every few months, as her lung function deteriorated. As a mom to young children, her lung function plummeted to 32%. She was evaluated for a lung transplant, but decided against it.
Her last ditch effort to save her lung function before having a lung transplant as the only option was to join a clinical trial for the Tobi Podhaler. Thus began her almost 20 year journey participating in various clinical trials. Since enrolling in her first trial, DeAnna’s lung function has increased from 32% to 58%.
When DeAnna joined her first trial, she wasn’t expecting much of anything out of it. She was simply going through the motions because she was so sick. She needed accountability, and the trial provided that, as well as additional care. She didn’t necessarily believe in what she was doing, but soon she found herself becoming increasingly invested. The care coordinator helped her to build relationships with a network of providers, and this is what it’s all about.
Now that DeAnna has participated in a variety of trials, her thoughts have changed. She believes that without clinical trials, she wouldn’t be here today.
Here is DeAnna’s advice for anyone who is considering participating in a clinical trial:
Do it. For yourself - see what is out there, what might work for you. For others - help your fellow person who cannot be in a trial.
This is how drugs come to market. Not only will you be able to help in that sense, but you will also garner connections and a community at local centers.
There is no downside to joining other than time invested in the study. Realistically, you can always quit, but you are going to get a more accurate understanding of where you are in the scheme of your condition. You will also get better care because you have more eyes on you.
If anything, she wishes she could go shout it to the world. Join a trial and contribute to research!
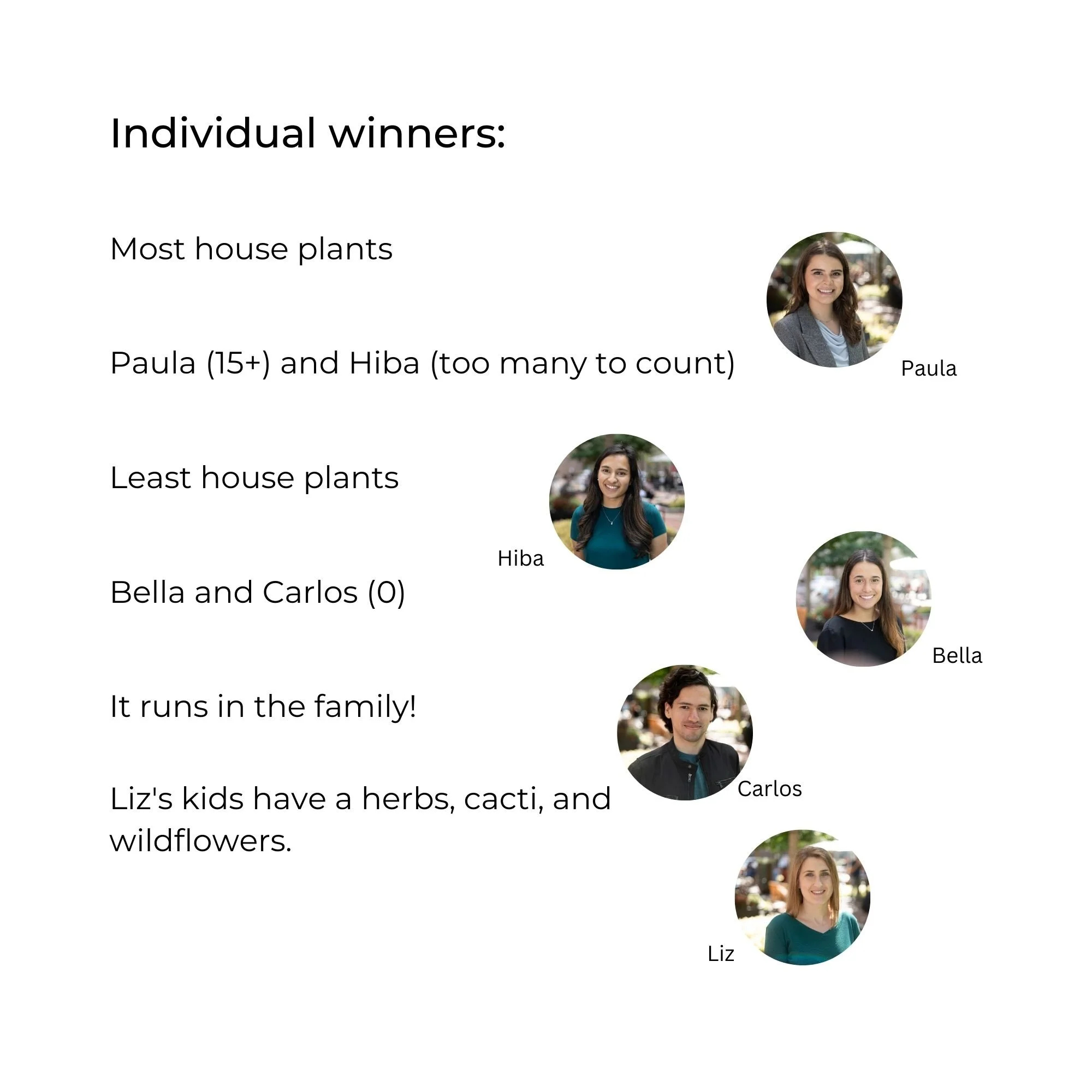
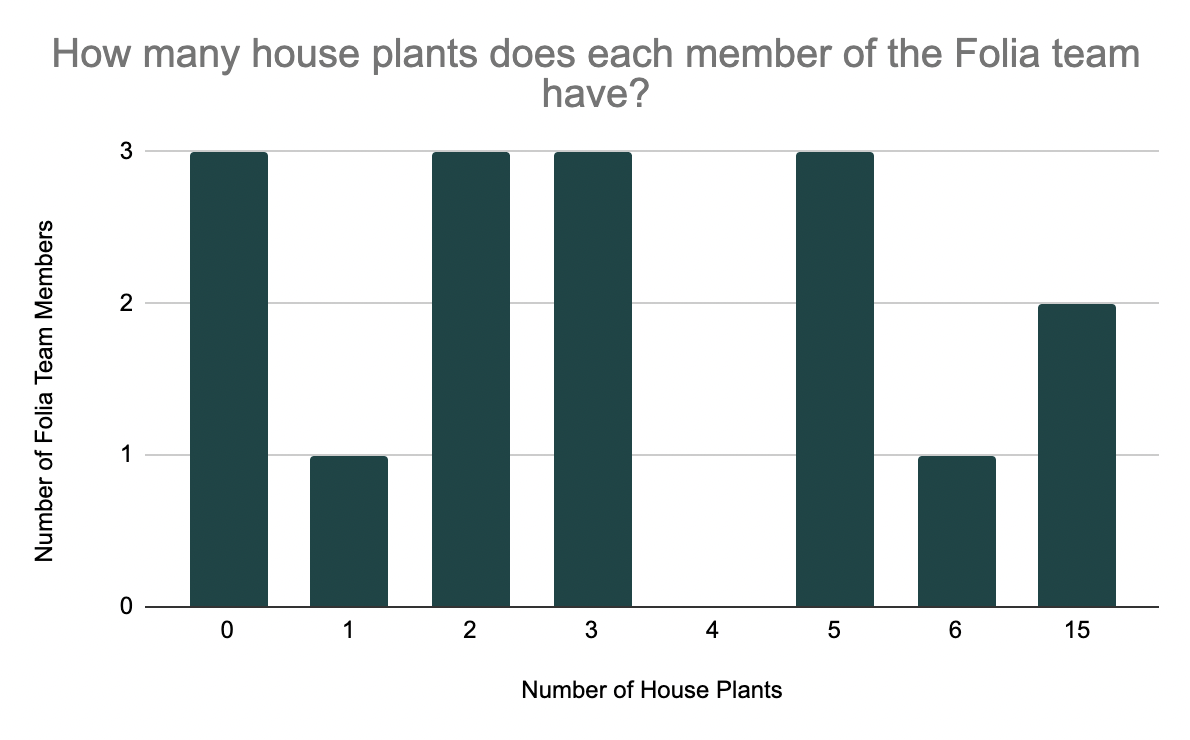
Folia Fun: Who has the biggest green thumb?
Folia Digest: What is a clinical trial?
Understanding the current clinical trial landscape
As of April 6, 2023, there were a total of 447,979 registered clinical trials occurring around the world (1). Since 2000, the number of registered studies has increased exponentially, and as science and technology continue to develop, the sky's the limit.
But what does it mean to join a clinical trial? Will you suddenly become a lab rat? We are here to help break it down, so you can better understand what it might be like to participate in a clinical trial.
Development of a treatment in the USA
The drug development process is long and drawn out, and is built in a way to keep humans safe. Step 1 of developing a treatment is Discovery and Development. Scientists will start researching everything they can about this new treatment in a laboratory. They test molecular compounds, explore new technologies, and draw insights into whatever they are discovering and trying to treat. Then, they reach Step 2, Preclinical Research. This is when a treatment undergoes laboratory and animal testing, so scientists can get a basic understanding of safety of the treatment. Once the treatment passes this step, it moves on to Step 3: Clinical research. This is the step we will be focusing on, as humans are introduced to the treatment. After a period of clinical research, the treatment goes through Step 4 - FDA review - where the FDA reviews all of the data from the trials, and decides whether to approve or deny the treatment. If approved, the treatment will move to Step 5 - FDA Post Market Safety Monitoring. The FDA will continue to monitor the safety of the treatment once it is on the market and available to the public (2).
What does this phase mean?
Say you are eligible to participate in a phase 2 clinical trial. This sounds exciting, but what does it actually mean? Each phase of a clinical trial is designed to uncover as much about the treatment/drug as possible, in as wide of a variety of individuals as possible.
A Phase 1 Clinical trial has about 20-100 individuals with the targeted condition. On average, the study lasts several months, and the main objective is to understand the safety and dosage of the treatment. If a treatment passes phase 1 - 70% of treatments do - then it moves on to Phase 2. A Phase 2 study will have up to several hundred people with the condition, and the study will last anywhere from several months to two years. The goal of this phase is to understand the efficacy and side effects. About 33% of treatments pass phase 2 and move on to phase 3.
A Phase 3 study has between 300 to 3,000 volunteer participants with the condition. The study will take about 1 - 4 years, and the purpose of this phase is to understand the efficacy of the treatment, and to monitor adverse/bad reactions. About 25-30% of treatments make it to Phase 4, and the population is expanded to several thousand individuals. The focus remains on the safety and efficacy of the treatment. Once all of the clinical trial steps are complete, the data is compiled and sent to the FDA for review (3).
Decentralized trials?
You might be familiar with the term “decentralized trials”. A fully decentralized trial is one where all procedures are done at home. A fully centralized trial is one where everything is done at the research site. Anything between these two opposites is considered a hybrid trial (4). Some drug companies might team up with an app (such as Folia!) to help them design a fully decentralized or hybrid trial. When considering participating in a clinical trial, this will be a major consideration, as centralized clinical trials require travel to and from the trial site.
Folia Logo Contest
In the last few months, we have been modifying the logo for each season. Whether it is adding a snowman for winter, or a flower for spring, we are enjoying seeing the variations of our Folia sprout.
This spring, our logo was created Dan's son, Aiden. We loved his creativity so much that we want to hold a Folia logo contest.
You can decorate our logo and submit your art for a chance to win $100!
Please go to our website at www.foliahealth.com/logocontest to learn more.
January 2023
First edition of the new year! Dives into POTS, a dysautonomic condition, and the pets of Folia! Scroll for the full edition.
Introducing: Dan
This quarter, we want to feature Dan. He is the Co-founder, CTO, and provider of music. He is also husband to his wife, Mercedes, and dad to his two kids Mila (11) and Aiden (7).
Dan's favorite part of working for Folia is that it allows him to help individuals on complex journeys. Up until Mila's birth, Dan had little exposure to the medical system. He and his wife felt they were suddenly on their own in an unfamiliar world. His inspiration at Folia comes from that feeling, as he knows how lonely and bewildering it is, and wants to help others in similar situations.
Outside of the office, Dan has a massive record collection with approximately 1500 records. He also DJs once or twice a year so he can share his records with friends.
A former runner, Dan enjoys being involved in his kid's athletic pursuits as their baseball and soccer coach. If he had a free weekend, he would spend it hanging out in the yard with his family, playing catch, and building a bonfire. However, he claims this would never happen. He is also a huge listener of Jojo Siwa, per Mila's recommendation.
This Quarter’s Latest News
Little insights into whats been happening at Folia!
Tracked! Reports
This example Tracked! graph shows the relationship between an individual's pain level and water
intake.
This winter, we introduced the Tracked! Reports. These customized reports are being hand delivered to individuals who requested them. They provide graphs and insights that go beyond the offerings of the app.
If you didn't sign up in time this year, don't worry! This new feature was more popular than we anticipated, and we are so excited to continue offering similar types of analysis in the future. If you requested a report and have yet to receive it, it is coming your way soon.
January Challenge
To kick off the year with positive habits, Liz, one of our program managers, launched the January Challenge. The goal of the challenge was to add something to a daily flow, track this action, and then pick and track a symptom that may be influenced by this new habit.
Members of the Folia community chose to drink more water, do 15 minutes of daily exercise, or try new incorporating new foods into their meals, and then track energy levels, acne, or mood. The combinations and possibilities are endless.
We are always trying to think of new ways to make trying new things fun, so if you have ideas about future challenges and community events, please let us know.
Upcoming: Community Conversations
In the past, we have used Community Conversations as an opportunity to connect with members of the Folia community, and share specific features of the app. We received some incredible feedback which inspired the next Community Conversations on Wednesday January 25 at 8 pm EST / 5 pm PST. We will be doing a demo for how to set up a profile from scratch, and how to customize it to fit your needs.
All are welcome, and the event is free. Please RSVP here so we can send you the zoom link.
Community Spotlight: Navigating a journey to diagnosis
We are so grateful for such a supportive and active core community. This week, we are excited to introduce Gretchen, a mom and businesswoman who has navigated a lengthy journey to diagnosis.
In 2015, at age 43, Gretchen finally received a diagnosis that was fitting of her symptoms: POTS. However, her health journey began over 25 years before this moment. In high school, Gretchen began to experience pre-syncope symptoms, typically as a result of heavy periods or standing up too quickly. Pre- syncope is the feeling you get before you are about to faint. The symptoms may include feelings of dizziness, nausea, general weakness, sweating, trouble hearing, or experiencing a visual “gray out”. Despite experiencing these symptoms, Gretchen didn’t have a supportive environment that would allow her to feel heard. She felt that without objective symptoms, she couldn’t say much.
In the five years leading up to her diagnosis, Gretchen was an active stay at home mom to two boys. Then, in February of 2015, she had a mild angioedema (swelling underneath the skin) with high blood pressure. Additionally, her heart rate was typically around 100 bpm, give or take.
At this point in time, she did not feel ready to accept blood pressure medication, so she started to document her symptoms.
She felt blessed to finally have a team of medical professionals that listened to her, and they started her on a path to diagnosis. By August of 2016, she was working part time, and was beginning to understand her limits, and how hard she can push herself.
By 2020, most of Gretchen’s POTS symptoms were under control, but she was struggling with GI issues, and how to go about finding solutions. Much to her dismay, she was advised by a care provider to begin the FODMAP diet. This diet is incredibly restrictive, and should not be practiced without the guidance of a medical professional. It cuts out a majority of common allergens, and then they are slowly reintroduced. While Gretchen wasn’t thrilled about this sudden lifestyle change, she went along with it, more because she wanted to “prove [the provider] wrong”. While Gretchen was right to a degree, she also found she is highly sensitive to gluten, fresh dairy, and any forms of garlic and onion. She continues to have GI issues, and speculates that they are related to the various autonomic aspects of a POTS diagnosis.
In July 2022, Gretchen watched the Dysautonomia Annual conference. She learned about new research, and practical daily living tips she didn’t previously know. She wishes she learned these tips back in 2015. She is back to juggling work, family, and her health, but this time with the help of knowledge, a strong support system, and of course, Folia.
Folia Fun: An objective ranking of the pets of Folia
From Left to right:
Most likely to be a Muppet: Fiona and Ollie
Class clown: Freeway and Walter
Asks to go outside at the worst times: Rosie and Julie
Is probably judging you right now (Clockwise starting with top right): Lemongrass Chicken aka LC, Sonoma (L), Stevie (R), Willow
Scientific Digest: What is POTS?
An estimated one to three million individuals in the United States are living with POTS. It typically affects adolescents, and symptoms can begin during puberty. If this condition is so prevalent, why is it so difficult to diagnose?
POTS stands for Postural orthostatic tachycardia syndrome. POTS can present as a wide range of symptoms that affect the body at various times. Additionally, the symptom that is most prevalent varies between individuals. (1) The average time to get a diagnosis is between 5 and 11 months. (2) Common symptoms of POTS include dizziness or lightheadedness, headaches, shaking and sweating, heart palpitations, fainting, brain fog, and poor sleep. POTS can also be characterized by a rise in heart rate of at least 30 bpm from sitting to standing position. A pale face and purple discoloration of limbs lower than the level of the heart are also hallmark symptoms of POTS. (3)
POTS is a condition that falls into a wider umbrella of conditions that are caused by issues with the autonomic nervous system (ANS). The ANS is the part of the nervous system that controls involuntary bodily functions. These functions aren’t consciously controlled, such as heart rate, breathing, digestion, or body temperature. (4) When the ANS doesn’t function properly, there can be issues with any of these internal systems, and it can cause issues with breathing, or blood pressure. Dysautonomia is the term for this group of conditions. Other dysautonomic conditions include diabetes, lupus, Sjogren’s syndrome and celiac disease.
POTS is a form of dysautonomia, and isn’t technically considered a disease, but instead it is a cluster of symptoms that typically present together. Because POTS isn’t a disease, it is thought to be caused by something else, and this adds to the delay in diagnosis. Most of the time, the root cause is not able to be figured out, and the symptoms are treated as they come. This type of POTS, where the root cause is unknown, is called Primary or Idiopathic POTS. POTS is considered to be secondary when another known medical condition is present, and contributes to POTS symptoms. (5)
One major risk factor for dysautonomia is having certain autoimmune diseases. (6) An autoimmune disease is when the body’s immune system attacks healthy cells. Recent research shows that POTS may actually be an autoimmune disease. In an article that was published this month, scientists and researchers share that the imbalance of antibodies in individuals with conditions such as POTS are giving them reason to believe that there is possible criteria to diagnose as an autoimmune ANS imbalance. (7)
Even though individuals with POTS experience symptoms such as memory loss, severe fatigue, and pain, laboratory and instrumental analyses aren’t able to detect any differences from normal or expected values. Furthermore, researchers believe that dysautonomic conditions might be associated with an imbalance of autoantibodies to G protein-coupled receptors (GPCRs).
GPCRs are found in almost every type of cell in the body. Patients with rheumatic diseases such as systemic lupus erythematosus or rheumatoid arthritis have concentrations of GPCRs that deviate from normal (either higher or lower concentrations). Clinically healthy individuals have a presence of anti-GPCR, and so if this natural production of anti-GPCR is altered in any way, then the development of autoimmune conditions may be triggered. Patients with POTS symptoms due to post-COVID syndrome were found to have an irregular number of anti- GPCRs. (8)
Nearly four years before this article was published, another group of researchers raised the same question, because they found that POTS is associated with elevated G-Protein coupled receptor autoantibodies. Their research is driven by the fact that POTS “is often misdiagnosed as chronic anxiety or a panic disorder because the autonomic failure in these patients is not severe”. Yet, living with POTS is a major shift in daily life.
This group of researchers collected detailed clinical symptoms of 55 patients diagnosed with POTS. They coupled these details with various blood tests to show the G-protein receptors in each individual. They observed that in most cases, patients with POTS have at least 1 elevated G-protein coupled adrenergic autoantibody. (9) In more simple terms, the evidence they collected supports their hypothesis that POTS may be an autoimmune disorder.
Because POTS has so many potential symptoms, it can be difficult to speak to a doctor or medical professional and feel understood. Here are a couple of tips for preparing for an appointment.
1.Take detailed notes on symptoms as they occur. Utilize your graphs and summaries to show objective measurements.
2.Print out a copy of all previous test results. 3.Prepare a list of questions you want to ask.
a.Example: If my anxiety/stress/depression is taken away, what medical condition might account for my symptoms? What tests would you run for these? (10)
If you don’t feel heard, it is okay to get another opinion.
Folia Community - you are wonderful, and we love hearing from you!
If you have any feedback, ideas for future stories, or want to be featured in a future edition of The Leaflet, please do not hesitate to reach out!
You can contact us via email - [email protected], on intercom, or through social media - @foliahealth on all platforms.
October 2022
An Introduction to The Leaflet. Including a community spotlight and recent happenings.